Health
Targeted Healing: The Future of Precision Medicine in Cancer Treatment

Cancer treatment has dramatically evolved over the years, moving from traditional approaches like chemotherapy and radiation to more advanced methods rooted in the intricacies of genetics and biology.
Precision medicine, which tailors treatment based on an individual’s genetic makeup and tumor profile, stands at the forefront of this revolution.
Precise medicines give hope for more effective and individualized treatment, perhaps increasing results and reducing side effects, by concentrating on the unique genetic alterations that cause cancer in each patient.
Understanding Precision Medicine in Oncology
Precision medicine in oncology leverages genetic, environmental, and lifestyle factors to customize treatment strategies. Each cancer case is unique, with distinct mutations and characteristics influencing how the disease develops and responds to therapy.
This personalized approach aims to dissect the various cancer types, identifying specific biomarkers that can guide treatment decisions.
According to a report from the National Cancer Institute, over 60% of oncology drugs approved from 2013 to 2018 targeted specific genetic mutations in tumors.
By understanding the molecular makeup of cancer cells, physicians can select therapies that have a higher probability of success for individual patients.
This personalized treatment pathway develops more effective outcomes and reduces the aggressive side effects typically seen with conventional treatments.
Targeting Genetic Mutations in Cancer
Targeting specific genetic mutations drives the success of precision medicine. Cancers often arise from mutations that alter key pathways for cell division and survival.
Mutations in genes like KRAS can lead to aggressive tumor growth and resistance to conventional therapies. Advancements in tumor genomic profiling allow oncologists to identify these alterations and develop treatment strategies accordingly.
The introduction of therapies such as monoclonal antibodies and small-molecule inhibitors highlights the transition towards mutation-specific treatments. One such promising innovation, the MRTX1133, is a Ras inhibitor of mutant KRAS G12D, which targets the prevalent KRAS G12D mutation found in many cancer types. These treatments reduce collateral damage to healthy cells and simultaneously improve therapy efficacy by focusing on these alterations.
Ongoing clinical trials are evaluating the safety and effectiveness of these targeted therapies in diverse patient populations. Combination strategies, pairing mutation-specific drugs with chemotherapy or immunotherapy, may further improve treatment outcomes.
Monitoring patients for emerging resistance mutations is critical to adjust therapeutic approaches quickly.
Personalized treatment plans increasingly rely on regular genomic assessments to track tumor evolution. The focus on genetic mutations offers hope for more effective, tailored cancer therapies with fewer side effects.
Clinical Trials and Their Impact on Precision Medicine
Clinical trials serve as the bedrock for establishing the efficacy of targeted therapies in precision medicine. As researchers continue exploring the vast genetic landscape of cancer, these trials provide critical insights into how specific treatments respond to various mutations.
Numerous clinical trials are focused on agents that inhibit mutated proteins associated with cancer development, aiming to bring forth new therapeutic options for patients.
Data revealed that patients enrolled in trials examining precision medicine strategies experience improved survival rates, highlighting the effectiveness of tailored treatments.
Innovative trial designs, including basket trials that evaluate drugs across multiple tumor types harboring the same mutation, further exemplify the adaptability of precision medicine.
The Role of Biomarkers in Tailored Treatments
Biomarkers play an important role in the implementation of precision medicine. These indicators provide critical information regarding how a patient’s cancer might behave and respond to specific treatments.
Biomarkers can be genetic mutations, proteins, or other factors measurable in a patient’s tumor or blood. Incorporating biomarker testing into cancer treatment strategies guarantees patients receive therapies matched closely to their tumors’ characteristics.
This approach aligns with the growing trend of biomarker-driven diagnostics, allowing for more accurate predictions of treatment efficacy.
The presence of PD-L1 or mismatch repair deficiency correlates with responsiveness to immunotherapy treatments.
By identifying such biomarkers, healthcare professionals can choose therapies that improve patient outcomes and reduce the likelihood of unnecessary side effects.

The Future, Challenges, and Opportunities
The future of precision medicine in cancer treatment is promising, but it faces several challenges. Advancements in genomic sequencing technologies allow for comprehensive tumor profiling, but accessibility and cost remain critical hurdles.
Guaranteeing equitable access to precision medicine for diverse populations continues to be a major challenge.
The complexity of cancer biology presents ongoing obstacles. Tumors can adapt and evolve, leading to resistance against targeted therapies.
To counter this, research must focus on combination therapies that can overcome resistance mechanisms. Addressing these challenges will unlock the full potential of precision medicine, creating new avenues for effective and durable cancer treatments.
Cancer treatment is rapidly transforming due to the emergence of precision medicine, which tailors therapy to the individual genetic makeup of patients.
Healthcare providers can provide patients with a more individualized treatment plan by focusing on particular genetic alterations and applying targeted medicines. Overcoming challenges related to access, cost, and resistance mechanisms can lead to more effective therapies and improved cancer outcomes for patients.

-
 Health6 days ago
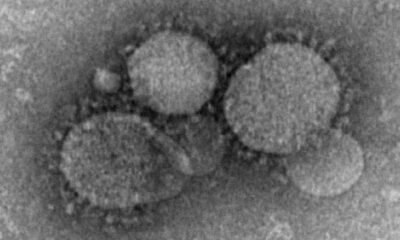
Health6 days agoFrance confirms 2 MERS coronavirus cases in returning travelers
-

 Health1 week ago
Health1 week ago8 kittens die of H5N1 bird flu in the Netherlands
-

 Entertainment6 days ago
Entertainment6 days agoJoey Valence & Brae criticize DHS over unauthorized use of their music
-

 US News3 days ago
US News3 days agoMagnitude 7.0 earthquake strikes near Alaska–Canada border
-

 Legal1 week ago
Legal1 week ago15 people shot, 4 killed, at birthday party in Stockton, California
-

 US News1 week ago
US News1 week agoFire breaks out at Raleigh Convention Center in North Carolina
-

 Legal5 days ago
Legal5 days agoWoman detained after firing gun outside Los Angeles County Museum of Art
-

 Health1 week ago
Health1 week agoEthiopia reports new case in Marburg virus outbreak