Reviews
Inpatient vs. Outpatient Rehab: What Will Your Insurance Pay For?

Choosing between inpatient and outpatient rehab is one of the most important decisions when seeking treatment for addiction. Each option provides different levels of care, and the right choice depends on an individual’s needs, the severity of their addiction, and their personal circumstances. However, cost is often a major concern, leading many to wonder what their insurance will cover.
Understanding the differences between inpatient and outpatient rehab, as well as how insurance providers handle coverage, can help individuals make informed decisions about their treatment.
Understanding Inpatient and Outpatient Rehab
Inpatient Rehab
Inpatient rehab, also known as residential treatment, requires individuals to stay at a facility for a set period. This type of rehab provides a highly structured environment with 24/7 medical supervision, therapy sessions, and support groups. It is often recommended for individuals with severe addictions, those with a history of relapse, or those who need a controlled setting to focus entirely on their recovery.
Since inpatient programs offer comprehensive care, they are generally more expensive than outpatient treatment. Costs can vary widely based on factors such as the length of stay, the facility’s amenities, and whether it is a private or state-funded center.
Outpatient Rehab
Outpatient rehab allows individuals to receive treatment while continuing to live at home. This option is typically best for those with mild to moderate addictions, strong support systems, or work and family commitments they cannot step away from. Outpatient programs include therapy sessions, group counseling, and medication-assisted treatment, but patients must manage their own schedules and maintain accountability.
Because outpatient treatment does not include residential accommodations or round-the-clock medical care, it is often more affordable than inpatient rehab. Many individuals choose outpatient programs when they need flexible treatment options that fit into their daily lives.
How Insurance Covers Inpatient and Outpatient Rehab
Most health insurance plans cover some level of addiction treatment, including both inpatient and outpatient care. The extent of coverage depends on the specific insurance provider, the policy details, and whether the treatment is deemed medically necessary.
Many insurance providers determine coverage based on:
- Medical necessity – Insurance companies may require an evaluation to determine whether inpatient care is essential or if outpatient treatment would be sufficient.
- Network restrictions – Some plans cover only in-network rehab facilities, while others provide partial coverage for out-of-network treatment.
- Length of treatment – Policies may have limits on how long they will cover inpatient stays or the number of outpatient sessions allowed.
What Will Your Insurance Pay For?
For individuals considering inpatient rehab, insurance may cover part or all of the treatment costs, but co-pays, deductibles, and out-of-pocket expenses will vary based on the policy. Some plans cover only a limited number of days, while others may require preauthorization before approving an extended stay.
Outpatient rehab is generally covered more extensively, as it is less costly for insurance providers. Many policies include coverage for therapy sessions, medication-assisted treatment, and support groups, making outpatient care an accessible option for many individuals. Those with United Healthcare insurance, for example, can explore their coverage options by checking with a United Healthcare rehab provider.
Verifying Insurance Coverage for Rehab
Before starting treatment, it is essential to verify insurance benefits to understand what costs will be covered. This process involves:
- Contacting the insurance provider to ask about coverage for inpatient and outpatient rehab.
- Speaking with the rehab facility to determine if they accept the insurance plan.
- Reviewing out-of-pocket expenses such as co-pays, deductibles, and coverage limits.
Finding the Right Treatment Plan
Choosing between inpatient and outpatient rehab depends on an individual’s specific needs, the severity of their addiction, and their financial situation. For those unsure about the best option, consulting with an addiction specialist can help determine the most effective course of treatment.
Rehab centers like United Recovery Project offer personalized treatment plans and assistance with insurance verification to help individuals navigate their options. Understanding what insurance will cover ensures that people seeking treatment can focus on recovery without the added stress of financial uncertainty.

-

 World1 week ago
World1 week agoEthiopian volcano erupts for first time in thousands of years
-

 Health2 days ago
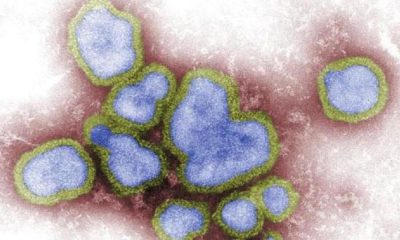
Health2 days ago8 kittens die of H5N1 bird flu in the Netherlands
-

 Legal7 days ago
Legal7 days agoUtah Amber Alert: Jessika Francisco abducted by sex offender in Ogden
-

 US News6 days ago
US News6 days agoExplosion destroys home in Oakland, Maine; at least 1 injured
-
 Health7 days ago
Health7 days agoMexico’s September human bird flu case confirmed as H5N2
-

 Legal3 days ago
Legal3 days ago15 people shot, 4 killed, at birthday party in Stockton, California
-

 World7 days ago
World7 days agoWoman killed, man seriously injured in shark attack on Australia’s NSW coast
-

 US News2 days ago
US News2 days agoFire breaks out at Raleigh Convention Center in North Carolina