Reviews
Driving Innovation in Healthcare Delivery Models

Healthcare delivery is transforming faster than ever, with systems adopting smarter, tech-driven approaches to meet the expectations of today’s patients. The focus is now toward models that combine efficiency with personalized care, giving people access to services when and how they need them. New tools and strategies are helping care teams streamline processes and improve overall outcomes in ways that weren’t possible just a few years ago.
Florida’s healthcare sector highlights both the challenges and possibilities of this shift. As one of the fastest-growing states, Florida serves a mix of urban and rural populations, seniors, and multicultural communities. These factors call for creative solutions to keep care accessible and effective. From leveraging telehealth to strengthening leadership in nursing, Florida providers are setting the stage for smarter, more adaptable care delivery models.
Empowering Nurses in Care Innovation
Nurses are at the center of these changes, often driving improvements in how care is delivered. As frontline professionals, they understand patient needs better than anyone, making them ideal leaders in efforts to reshape healthcare systems. Giving nurses more influence in decision-making helps organizations create care models that are practical, responsive, and patient-focused.
Supporting this leadership requires access to advanced education. For this purpose, online nursing programs in Florida offer an efficient way to expand their skills and prepare for bigger roles. Programs like those at St. Thomas University are leading the way by offering flexible, high-quality learning that fits into busy work schedules. Nowadays, working nurses often prefer online programs because they allow them to grow professionally without stepping away from their roles, combining convenience with strong academic support.
Using Data to Predict Needs
Predictive analytics is quickly becoming an essential part of healthcare innovation. By analyzing data on patient histories, care trends, and health outcomes, providers can spot risks early and take proactive steps.
Hospitals and clinics are adopting such tools to better understand their populations and anticipate demand. When paired with insights from nursing teams, analytics systems can guide smarter staffing, improve patient safety, and help reduce avoidable readmissions.
Coordinating Patient-Centered Care
Putting patients at the center of care has become a defining trend in healthcare. Instead of rigid systems, modern models emphasize collaboration, communication, and individualized treatment plans. This shift helps patients feel more engaged in their health while improving outcomes for providers.
In regions where cultural and language diversity is significant, patient-centered care models are especially important. Nurses play a major role here by serving as connectors between patients and larger care teams.
Building Value-Based Frameworks
Healthcare organizations are moving toward value-based frameworks that reward results instead of the number of procedures performed. These systems encourage preventative care, efficient use of resources, and better long-term outcomes.
Value-based models are helping reduce care gaps while supporting a healthier population. Nurses and interdisciplinary teams collaborate under these frameworks to track progress, adjust plans quickly, and focus on quality care. This approach aligns with national trends while addressing the state’s unique healthcare needs.
Expanding Telehealth Services
Telehealth has evolved into a core part of healthcare delivery, making it easier for patients to connect with providers without geographic barriers. Virtual consultations, remote monitoring, and digital check-ins give patients more flexibility while allowing providers to reach those who might otherwise skip routine care.
For care teams, telehealth also improves efficiency. Nurses and physicians can manage follow-ups, monitor chronic conditions, and respond quickly to concerns without the need for in-person visits.
Optimizing Resources in Underserved Communities
Communities with limited access to medical services face ongoing challenges in getting the care they need. Minimizing these gaps means making smarter decisions about how resources are distributed and using technology to fill in the gaps where staff or facilities may be scarce.
Care teams are finding ways to bring services directly to these areas through mobile health units, community-based programs, and better supply chain management. Such effective strategies reduce disparities and help create a more balanced healthcare system for everyone.
Enhancing Patient Education with Digital Tools
Digital tools are becoming key in helping patients better understand and manage their health. Mobile apps, interactive platforms, and virtual resources give people the knowledge to make informed decisions about their care.
Nurses often lead these efforts, using digital platforms to teach patients about medications, lifestyle changes, and chronic disease management. This approach promotes self-care and empowers patients to take charge of their well-being between appointments.
Leveraging AI in Care Teams
Artificial intelligence is no longer just a buzzword; it’s transforming how healthcare teams work. From predictive analytics to virtual assistants, AI supports decision-making by analyzing massive amounts of data and presenting actionable insights.
Care teams use AI to identify patterns, flag potential complications, and recommend treatment adjustments. Nurses benefit from these tools as they streamline workflows, minimize repetitive tasks, and give providers more time to focus on patients.
Adapting Care for Rural Areas
Delivering healthcare in rural regions requires flexible models that can overcome distance and infrastructure challenges. Mobile clinics, telehealth networks, and collaborative partnerships with local organizations are helping extend services into these harder-to-reach places.
Care delivery models built for rural areas often focus on prevention, chronic disease management, and easy access to primary care. Nurses play an important role in these systems by building trust within communities and coordinating care that fits local needs.
Healthcare delivery is moving into a new era where innovation, technology, and leadership work hand in hand to create better experiences for patients and providers alike. From empowering nurses to implementing AI, these strategies are reshaping how care is provided. The focus remains on building systems that are adaptable, efficient, and centered on the people they serve.

-

 World1 week ago
World1 week agoEthiopian volcano erupts for first time in thousands of years
-

 Health2 days ago
Health2 days ago8 kittens die of H5N1 bird flu in the Netherlands
-

 Legal7 days ago
Legal7 days agoUtah Amber Alert: Jessika Francisco abducted by sex offender in Ogden
-

 US News6 days ago
US News6 days agoExplosion destroys home in Oakland, Maine; at least 1 injured
-
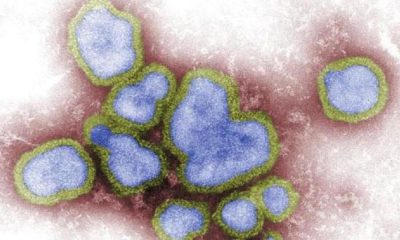
 Health7 days ago
Health7 days agoMexico’s September human bird flu case confirmed as H5N2
-

 Legal3 days ago
Legal3 days ago15 people shot, 4 killed, at birthday party in Stockton, California
-

 World7 days ago
World7 days agoWoman killed, man seriously injured in shark attack on Australia’s NSW coast
-

 Health6 days ago
Health6 days agoMarburg outbreak in Ethiopia rises to 12 cases and 8 deaths