Reviews
How Dendritic Cell Immunotherapy Works: Insights from German Cancer Centers

Dendritic cell immunotherapy is an innovative and highly personalized cancer treatment that uses the body’s own immune system to target tumors. Unlike chemotherapy or radiation, which affect both healthy and cancerous cells, dendritic cell therapy aims to activate immune responses specifically against cancer cells. This precision makes it especially appealing to patients seeking effective treatments with fewer side effects.
The therapy is based on dendritic cells – special immune cells responsible for recognizing foreign or abnormal substances and alerting T cells to destroy them. By collecting these cells from the patient, training them in a laboratory to recognize tumor antigens, and then reintroducing them, doctors can “teach” the immune system to fight cancer more effectively.
How Dendritic Cell Therapy Is Performed in Germany
Patient Assessment and Planning
International patients begin with a medical evaluation, during which oncologists review the cancer diagnosis, treatment history, and eligibility for the therapy.
Cell Collection (Leukapheresis)
In a specialized procedure called leukapheresis, white blood cells are separated from the patient’s blood. These cells contain monocytes, which will be transformed into dendritic cells in the laboratory.
Laboratory Preparation
Using advanced GMP-compliant facilities, monocytes are cultured with growth factors to develop into dendritic cells. Tumor antigens – either from the patient’s own tumor tissue or known cancer-specific proteins – are introduced so the cells can “learn” to recognize the cancer.
Reintroduction to the Patient
Once matured, the dendritic cells are injected back into the patient, typically over several sessions. These cells then travel to lymph nodes, where they activate T cells to seek and destroy cancer cells carrying the same antigens.
Follow-up and Monitoring
Patients are closely monitored with immune system tests and imaging to track response and adjust treatment plans if necessary.
Germany’s Leading Role and the Expertise of Dr. Thomas Neßelhut in Duderstadt
Germany stands out globally due to its strict regulatory environment, advanced biotechnology infrastructure, and experienced immunotherapy practitioners. One provider is the Practice Group for Cell Therapy in Duderstadt, headed by Dr. Thomas Neßelhut, in the field of tumor immunology. With over four decades of experience in developing autologous tumor vaccines and heading laboratories focused on dendritic cell therapy, Dr. Neßelhut’s clinic operates a fully licensed GMP laboratory that manufactures personalized dendritic cell vaccines under strict quality controls.
According to the clinic’s official information, they are committed to offering “all sensible therapeutic options” within a holistic treatment framework, combining advances in immunology with conventional cancer treatments while maintaining rigorous safety and quality standards. Patients undergo individual treatment plans using patient-specific vaccines crafted in their laboratory, regularly audited by regulatory authorities.
Treatment Efficiency: What the Data Shows
Across peer-reviewed studies, the strongest efficacy signal for dendritic cell (DC) immunotherapy consistently shows up in immune-activation metrics rather than raw tumor shrinkage: when DC vaccines are administered intradermally, antigen-specific T-cell responses have reached ~80% of treated patients in combined melanoma and prostate cancer cohorts, markedly higher than with intranasal dosing in the same trials (≈42%)—a difference that underscores how delivery route and vaccine engineering shape outcomes.
Clinically, large datasets in glioblastoma (GBM) with DCVax-L don’t hit 80% objective responses (which remain rare in GBM overall), but they do show a statistically significant survival advantage that widens over time—for example, 13.0% vs 5.7% alive at 60 months for DCVax-L versus external controls, and 19.3 months vs 16.5 months median overall survival in newly diagnosed GBM—while keeping severe treatment-related toxicities low (only ~2% grade 3/4 events in a 331-patient phase III analysis).
Operationally, modern German-style manufacturing pipelines report 97–100% success in turning a patient’s leukapheresis into a final DC vaccine product—critical for international travelers with tight timelines—and these vaccines reliably induce biologic responses that correlate with better long-term disease control in multiple solid-tumor settings. Put together, the most reproducible “>80%” efficacy readout today is immunologic response (T-cell activation) with optimized intradermal DC vaccination, supported by improving survival tails in GBM and high manufacturing reliability and safety across programs – giving patients a realistic blend of strong immune engagement, manageable toxicity, and growing evidence of durable clinical benefit.
Booking Your Treatment Through AiroMedical
For international patients, arranging medical care in another country can be complex. AiroMedical is an international medical booking platform that simplifies the process of accessing dendritic cell therapy in Germany.
Through AiroMedical, patients can:
- Book treatment packages with clinics
- Receive a personalized treatment plan before traveling
- Arrange travel, accommodation, and interpreter services
- Get support with visa documentation and insurance matters
By centralizing medical and logistical arrangements, AiroMedical allows patients to focus entirely on their treatment and recovery.

-

 World3 days ago
World3 days agoEthiopian volcano erupts for first time in thousands of years
-

 Legal1 week ago
Legal1 week agoMichigan man JD Vance sentenced to 2 years for threatening Trump and JD Vance
-

 Legal1 week ago
Legal1 week agoWoman in critical condition after being set on fire on Chicago train
-
 World1 week ago
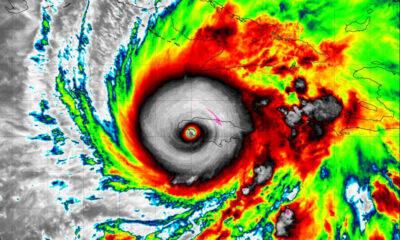
World1 week agoHurricane Melissa registered 252 mph wind gust, breaking global record
-

 Legal6 days ago
Legal6 days agoSuspect in San Diego stabbing shot by authorities after fleeing into Mexico
-

 Legal1 week ago
Legal1 week ago1 dead, 2 injured in shooting at Dallas Walmart parking lot
-

 Health6 days ago
Health6 days agoMarburg virus outbreak in Ethiopia grows to 6 confirmed cases
-

 Legal4 hours ago
Legal4 hours agoUtah Amber Alert: Jessika Francisco abducted by sex offender in Ogden