Reviews
Why Nursing Continues to Lead in Patient-Centered Care

Ever been in a hospital bed wondering who to talk to? Specialists come and go. Charts pile up. But the one person who always seems to have answers—and time—is the nurse. From late-night check-ins to calmly explaining unfamiliar terms, nurses connect the dots and humanize the whole experience. Long before “personalized care” became trendy, they were already doing it. Nursing didn’t adopt patient-centered care—it defined it.
In this blog, we will share why nursing continues to lead in patient-centered care, how it adapts to modern challenges, and why its role matters more than ever in an increasingly complex world.
Nurses Stay Close to the Story
Nurses don’t just show up—they stay present. While doctors often assess and move on, nurses remain at the bedside, noticing shifts in both physical and emotional health. They see more than charts; they see people navigating pain, fear, and recovery.
This constant presence matters. Patients often feel lost in the medical shuffle. Nurses step in as translators and companions, helping patients understand what’s happening and why it matters. That connection can make the difference between treatment compliance and confusion.
Recovery isn’t just clinical—it’s personal. Nurses make sure patients eat, sit up, and feel supported. Their care covers what machines and procedures can’t: the everyday details that help people heal.
Training That Focuses on the Whole Person
Treating issues in isolation doesn’t work. Nurses are trained to collaborate with other professionals and ask meaningful questions like “Do you have support at home?” or “Can you afford your medication?” These insights help them deliver care that fits real lives.
And the education doesn’t stop after graduation. Many nurses choose to grow their skills through advanced degrees. An online masters of nursing program allows working professionals to dive deeper into leadership, informatics, or care coordination—while still staying in the field. These programs open doors without closing off flexibility, letting nurses build expertise that strengthens the care they give and the systems they work in.
It’s not just about moving up the career ladder. It’s about understanding care on a deeper level—what it means, how it’s delivered, and how it can reach more people.
Responding to Real-World Crises
Remember the early days of the COVID-19 pandemic? Hospitals were overwhelmed. Ventilators were scarce. Families weren’t allowed to visit. And yet, it was nurses who stayed beside patients, often holding their hands when no one else could. If you want to know what patient-centered care looks like under pressure, that was it.
But even beyond the pandemic, nurses have shown time and again they’re not just part of the system—they hold it up when it starts to wobble. During natural disasters, public health emergencies, or mass casualty events, they’re often the first to act and the last to rest.
And in everyday care, especially in rural or underserved communities, nurses fill gaps that no one else does. They conduct home visits, follow up with discharged patients, and advocate for basic needs like food or housing. While systems lag, nurses show up.
The Rise of Personalized Care—and the Nurse’s Role in It
Medicine is becoming more personalized. With genetic testing, AI, and electronic health records, we can tailor treatments like never before. But here’s the catch: the best data in the world won’t matter if no one helps the patient make sense of it.
Nurses translate complex information into real-life decisions. They explain side effects in plain language. They listen to patients’ goals. They help create plans that match real circumstances—not just textbook recommendations.
They also ask the most human question in healthcare: “What matters to you today?”
This simple question often unlocks deeper insights. Maybe a patient’s main worry isn’t their cholesterol—it’s how to keep caring for their grandkids while recovering. Nurses don’t dismiss that concern. They build care around it.
That’s where patient-centered care really lives: not in data points, but in details that only listening can reveal.
The Trust Patients Lean On
Trust doesn’t come from credentials alone—it’s earned moment by moment. And in healthcare, nurses are consistently ranked among the most trusted professionals for a reason. They’re not just executing orders; they’re listening, observing, and often catching what others miss. Patients tend to share more with the person who checks in at 3 a.m. than the one who stops by for five minutes with a clipboard.
This trust becomes the backbone of advocacy. Nurses speak up when something feels off, even if the chart looks fine. They question prescriptions that don’t make sense for a patient’s lifestyle. They notice side effects that a patient didn’t know were worth mentioning. When decisions get complicated or overwhelming, nurses help patients navigate them with clarity and confidence.
Where We Go From Here
Patient needs aren’t getting simpler. We’re dealing with aging populations, rising mental health challenges, and deepening inequalities in access to care. The solution isn’t just better drugs or faster systems. It’s better relationships.
And that’s what nursing has always delivered.
To keep leading in patient-centered care, the profession needs more support—more funding, more seats at the leadership table, and more recognition of the invisible labor that drives real outcomes. It’s not just about giving medicine. It’s about giving attention.
The future of healthcare depends on how well we remember this: healing starts when people feel seen. And the people best at making that happen have been doing it all along—in scrubs, in sneakers, with a clipboard in one hand and compassion in the other.
If we’re serious about making care truly centered on the patient, then we need to stop thinking of nursing as the supporting act. It’s the heart of the show.
All in all, it’s tempting to think of healthcare as a tech puzzle or a numbers game. But no device or algorithm can replace what happens when someone listens, really listens, and adjusts care to fit your life—not just your chart.
Nursing doesn’t chase trends. It responds to need.
That’s why, in an industry full of change, this one truth holds steady: if you want to understand how care should feel, look at what nurses are already doing. Patient-centered care isn’t a strategy to them. It’s just Tuesday.
And maybe that’s the point.

-

 World3 days ago
World3 days agoEthiopian volcano erupts for first time in thousands of years
-

 Legal1 week ago
Legal1 week agoMichigan man JD Vance sentenced to 2 years for threatening Trump and JD Vance
-

 Legal1 week ago
Legal1 week agoWoman in critical condition after being set on fire on Chicago train
-
 World1 week ago
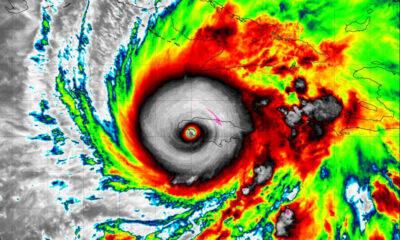
World1 week agoHurricane Melissa registered 252 mph wind gust, breaking global record
-

 Legal6 days ago
Legal6 days agoSuspect in San Diego stabbing shot by authorities after fleeing into Mexico
-

 Legal1 week ago
Legal1 week ago1 dead, 2 injured in shooting at Dallas Walmart parking lot
-

 Health6 days ago
Health6 days agoMarburg virus outbreak in Ethiopia grows to 6 confirmed cases
-

 Legal6 hours ago
Legal6 hours agoUtah Amber Alert: Jessika Francisco abducted by sex offender in Ogden