Reviews
Decoding Disease Transmission: A Look at How Infectious Diseases Spread

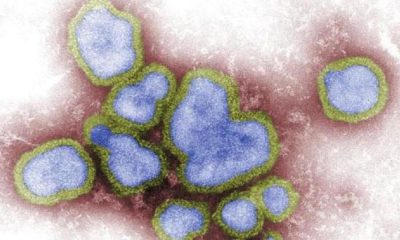
Infectious diseases have profoundly shaped human history, causing pandemics, altering the course of societies, and driving major advancements in medicine and public health. But how do these diseases spread from one person to another? Understanding disease transmission is key to prevention.
This article will discuss the various modes of transmission, explore how everyday actions influence disease spread, and highlight the importance of protective measures, especially for those working in high-risk environments such as the healthcare sector.
What is disease transmission?
Disease transmission refers to the process by which an infectious agent, like a virus, bacterium, or parasite, moves from one host to another. The success of this transfer depends on several factors, including the type of pathogen, the environment, and the behavior of the people involved.
How diseases are spread
Transmission routes are typically grouped into five major categories: direct contact, indirect contact, droplet, airborne, and vector-borne. Each comes with its own set of challenges when it comes to containment and prevention. Let’s discuss the five categories in more detail below:
Direct contact transmission
Direct transmission occurs when a pathogen is transferred through physical contact between people. This includes activities like hugging, kissing, touching open wounds, or sexual contact.
Common diseases spread through direct contact include herpes, the simplex virus, HIV/AIDS, and staph infections. Prevention in this case often involves simple hygiene practices, such as frequent handwashing and using protection during sexual activity.
Indirect contact transmission
This type of transmission occurs when a person touches a surface or object (called a fomite) that an infected person has contaminated. Door handles, elevator buttons, mobile phones, and shared medical equipment are all potential culprits.
For instance, if someone with the flu sneezes into their hand and then grabs a doorknob, the next person who touches that doorknob could pick up the virus. To reduce risk, clean and disinfect commonly touched surfaces regularly, avoid touching your face, especially eyes, nose, and mouth, and use gloves and disposable tools in clinical settings.
Droplet transmission
Many respiratory illnesses, including the flu, common cold, and most recently, COVID-19, are spread via droplets. These are small particles that are expelled when someone coughs, sneezes, or even talks. The droplets can land on nearby individuals or surfaces.
Droplet transmission typically occurs within six feet of the source, which is why social distancing and wearing masks are effective protective measures.
Airborne transmission
Unlike droplet transmission, airborne diseases can linger in the air for extended periods and travel over longer distances. These pathogens are carried by microscopic particles that can be inhaled deep into the lungs. Examples include tuberculosis, measles, and chickenpox.
Because airborne diseases are harder to contain, prevention often requires enhanced ventilation, air filtration systems, and N95 respirators in healthcare settings.
Vector-borne transmission
Vectors are living organisms, often insects, that carry and transmit infectious pathogens to humans. Common vectors include mosquitoes that carry Zika virus, malaria, and West Nile virus; ticks that pass on Lyme disease or Rocky Mountain spotted fever; and fleas that can transmit plague.
Preventing vector-borne disease often involves using insect repellent, wearing protective clothing, and controlling breeding grounds for mosquitoes and other carriers.
Infection prevention in high-risk settings
People working in healthcare environments are particularly vulnerable to infectious disease exposure due to frequent contact with ill patients, contaminated materials, and invasive procedures.
Hospitals and clinics implement strict infection control protocols, including the use of personal protective equipment such as gloves, gowns, and masks, hand hygiene policies, isolation procedures for contagious patients, as well as vaccination requirements for staff. These precautions are not only vital for the safety of patients but also for protecting the frontline workers themselves.
This is where advanced nursing education comes into play. Nurses with specialized training are better equipped to identify transmission risks, apply evidence-based practices, and lead infection control initiatives. Those looking to enhance their qualifications might consider enrolling in online post masters NP programs that offer the flexibility to balance work and study while gaining clinical expertise.
Everyday actions that make a difference
Infection control isn’t just for hospitals. It’s something we all play a role in. Here are a few simple but powerful ways to help stop disease transmission in daily life:
- Stay home when you’re sick
- Cover your mouth and nose when coughing or sneezing
- Wash hands thoroughly for at least 20 seconds
- Get recommended vaccines and booster shots
- Clean and disinfect frequently used surfaces
- Avoid sharing personal items like towels, razors, and utensils

Understanding how infectious diseases spread gives us the tools we need to prevent them. Whether it’s something as simple as covering a cough or as complex as managing hospital-wide infection control programs, every action counts.
For healthcare professionals, staying informed and pursuing continued education is crucial in the fight against disease transmission. By investing in advanced training and remaining vigilant in daily practices, we can create safer environments for everyone, from hospital patients to families at home.

-

 World1 week ago
World1 week agoEthiopian volcano erupts for first time in thousands of years
-

 Health2 days ago
Health2 days ago8 kittens die of H5N1 bird flu in the Netherlands
-

 Legal7 days ago
Legal7 days agoUtah Amber Alert: Jessika Francisco abducted by sex offender in Ogden
-

 US News6 days ago
US News6 days agoExplosion destroys home in Oakland, Maine; at least 1 injured
-
 Health7 days ago
Health7 days agoMexico’s September human bird flu case confirmed as H5N2
-

 Legal3 days ago
Legal3 days ago15 people shot, 4 killed, at birthday party in Stockton, California
-

 World7 days ago
World7 days agoWoman killed, man seriously injured in shark attack on Australia’s NSW coast
-

 Health6 days ago
Health6 days agoMarburg outbreak in Ethiopia rises to 12 cases and 8 deaths