Reviews
How Will 2026 Coding Updates Affect Pain Management Billing Services?
Several coding changes taking effect in 2026 will change how clinics bill for pain care. This short guide explains what those updates mean for pain management billing services and what billing teams should do first. It covers new and revised CPT and HCPCS codes, RPM/RTM expansions, PLA lab entries used for pharmacogenomics, and ICD-10 sequencing guidance that affects pain claims. Each item focuses on practical impact: documentation, charge capture, prior authorization, and denials. Use the checklist that follows to spot risk areas and update your workflows before the new rules take effect.
Which 2026 Coding Changes Will Have the Greatest Impact on Pain Management Billing Services?
Several updates announced for 2026 touch different parts of the billing cycle, but a few stand out because they change how pain procedures, remote monitoring, and diagnoses are recorded. These areas are the ones most likely to affect accuracy, reimbursement, and audit risk, which is why they are broken down in the sections below:
How Will New CPT Codes Change Reporting for Pain Procedures and Monitoring?
The 2026 CPT updates introduce several new and revised codes that directly affect pain management billing services. Below is a summary of the key code changes:
| CPT / RTM Code | Description | Change for 2026 |
| 99445 | RPM: device supply/data, 2–15 days | New code |
| 99470 | RPM: treatment-management, first 10 min | New code |
| 98984 | RTM device/data, 2–15 days | New code |
| 98985 | RTM device/data, 2–15 days | New code |
| 98986 | RTM device/data, 2–15 days | New code |
| 98979 | RTM treatment-management, first 10 min | New code |
| 64567 | Percutaneous electrical nerve field stimulation (PENFS, cranial nerves, without implantation) | New Category I code replaces 0720T |
These 2026 code changes allow pain management practices to capture short-duration remote monitoring and therapeutic management that was previously unbillable, while providing a standardized way to report PENFS procedures. The updates improve revenue capture for brief monitoring episodes, post-procedure follow-ups, and non-implant neuromodulation treatments.
What HCPCS Adjustments Are Expected for Neurostimulation and Device Billing?
For 2026, HCPCS Level II updates introduce one key code relevant to pain management: C1607, which identifies implantable integrated neurostimulator devices. This new code replaces any previous generic coding and standardizes reporting for neuromodulation implants.
Billing teams must update device master files, claim templates, and documentation workflows to include C1607 where applicable. Proper use ensures accurate reimbursement, aligns implant procedures with payer requirements, and reduces the risk of claim denials or miscoding for spinal cord or peripheral nerve stimulators.
How Do FY-2026 ICD-10-CM Revisions Affect Pain Diagnoses and Sequencing?
The FY‑2026 ICD‑10‑CM update brings new codes and changes affecting how pain, especially abdominal, pelvic, perineal, and chronic, is documented and billed. Below are the key changes for pain management:
| Change Description | What It Adds or Revises (Pain‑Relevant) |
| More granular codes for abdominal, pelvic, and perineal pain | 16 new symptom codes for abdominal/pelvic/perineal pain and tenderness |
| Broad expansion: 487 new codes overall | FY‑2026 adds 487 new codes, some relevant to pain or comorbid conditions |
| Updated sequencing rules for pain vs. site-specific diagnoses | Guidelines clarify whether to list G89 (pain) or site-specific/device pain first depending on the encounter |
New symptom codes allow precise documentation of pain location and type, supporting clinical necessity and payer review. Sequencing rules clarify whether to list G89 or site-specific codes first
How Will Remote Monitoring Updates Influence Pain-Care Workflows in 2026?
The 2026 updates introduce new short-duration RPM and RTM codes, including 99445, 99470, 98984to 98986, and 98979, allowing billing for 2 to 15 days of monitoring and 10-minute management sessions. Pain clinics can now capture brief post-procedure follow-ups, therapy adherence, and home monitoring that were previously unbillable.
Billing teams must revise charge masters, coding workflows, and documentation templates. Similarly, clinicians should record monitoring duration and patient interactions accurately to ensure correct reimbursement and reduce denials. These updates streamline reporting and support more efficient pain-care workflows.
How Should Billing Teams Prepare for Upcoming Prior Authorization Shifts?
In 2026, many payers are expanding prior authorization for interventional pain procedures, neuromodulation implants, and certain pharmacogenomic tests. Billing teams should proactively track which CPT, HCPCS, and PLA codes require authorization, update clearinghouse edits, and maintain a payer-policy tracker. Coordinating with clinical staff to submit complete documentation before procedures will reduce denials. Teams must also educate providers on any new PA requirements to ensure timely approvals and smooth workflow, minimizing interruptions in patient care and revenue cycle delays.
What Steps Can Clinics Take Now To Reduce Denials Before the 2026 Updates Go Live?
Before 2026 updates take effect, pain clinics can adopt proactive measures to reduce claim denials and ensure smooth billing for new codes, monitoring, and prior authorization requirements.
1. Review and Update Coding Templates
Audit current EHR templates to include all 2026 CPT, HCPCS, RTM, and ICD-10 updates. This ensures accurate coding for pain management and reduces claim rejections.
2. Train Staff on Code Changes
Provide clinical and billing teams with training on new codes and documentation requirements. This improves reporting accuracy and minimizes errors in claim submission.
3. Implement Pre-Authorization Workflows
Update workflows to handle expanded prior authorization for interventional procedures and device-based pain services. Ensure approvals are obtained before patient care to prevent delays.
4. Monitor Payer Policy Updates
Track changes in payer rules for RPM, RTM, neurostimulators, and pharmacogenomic tests. Staying updated allows billing teams to adjust claims and avoid denials.
5. Outsource to Dedicated Billing Companies
Partner with experts like Transcure for complex coding, prior authorizations, and claim management. This streamlines processes, improves accuracy, and ensures timely reimbursement.
Conclusion
The 2026 coding, remote monitoring, device, and prior authorization updates will significantly impact pain management billing services. Clinics that proactively update templates, train staff, monitor payer rules, and consider outsourcing to experts like Transcure can reduce denials and ensure accurate, timely reimbursement. Preparing now helps practices adapt smoothly to these changes while maintaining efficient pain-care workflows.

-
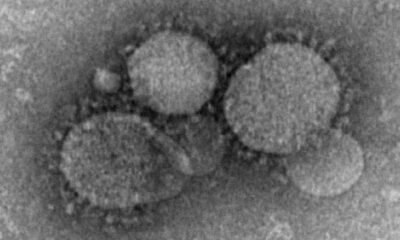
 Health1 week ago
Health1 week agoFrance confirms 2 MERS coronavirus cases in returning travelers
-

 US News6 days ago
US News6 days agoMagnitude 7.0 earthquake strikes near Alaska–Canada border
-

 Entertainment1 week ago
Entertainment1 week agoJoey Valence & Brae criticize DHS over unauthorized use of their music
-

 Legal3 days ago
Legal3 days agoShooting at Kentucky State University leaves 1 dead and another critically injured
-

 Legal1 week ago
Legal1 week agoWoman detained after firing gun outside Los Angeles County Museum of Art
-

 Business2 days ago
Business2 days agoUnpublished TIME cover suggests AI leaders may be named Person of the Year
-

 Health1 week ago
Health1 week agoEthiopia reports new case in Marburg virus outbreak
-

 Entertainment1 week ago
Entertainment1 week agoSeveral countries withdraw from 2026 Eurovision after Israel is allowed to participate